Cardiovascular medications
Anti-hypertensives
In general, continue these anti-hypertensive medications on morning of surgery.
ACE inhibitors / ARBs
These should be continued as normal pre-operatively.
Examples:
- ACEi: Captopril, Enalapril, Fosinopril, Imidapril, Lisinopril, Perindopril, Quinapril, Ramipril, Trandolapril
- ARB: Azilsartan, Candesartan, Eprosartan, Irbesartan, Losartan, Olmesartan, Telmisartan, Valsartan
- Combination: Valsartan/Sacubitril (Entresto®)
Beta blockers
Continue beta-blocker medications pre-operatively. For patients on sotalol, check potassium and magnesium levels pre-operatively if a U&E is indicated1.
Examples: Acebutolol, Atenolol, Betaxolol, Bisoprolol, Carvedilol, Celiprolol, Labetalol, Levobunolol, Metoprolol, Nadolol, Nebivolol, Pindolol, Propranolol, Sotalol, Timolol
Calcium channel blockers
Continue calcium channel blocking drugs as normal.
Examples: Dihydropyrodines: Amlodipine, Felodipine, Lacidipine, Lercanidipine, Nicardipine, Nifedipine, Nimodipine, Diltiazem, Verapamil
Vasodilators
These should be continued as normal pre-operatively.
Examples: Hydralazine, Minoxidil
Diuretics
Loop diuretics
Loop diuretics should be held on the morning of surgery unless the patient has heart failure and gentle physical activity causes fatigue, palpitations, or dyspnoea (i.e. METS < 4 due to heart failure)
This includes certain combinations (below).
Examples: Bumetanide, Furosemide, Torasemide, Bumetanide + Amiloride, Co-amilofruse, Furosemide + Spironolactone, Furosemide + Triamterene, Furosemide + Potassium Chloride
Potassium-sparing
Continue these drugs in the pre-operative period, even if part of a combination.
Examples: Amiloride, Eplerenone, Spironolactone, Triamterene, co-amilofruse, co-amilozide, amiloride + bumetanide, spironolactone + furosemide, Kalspare®, amiloride + hydrochlorothiazide + timolol, co-flumactone, co-triamterzide
Thiazides
Continue these drugs in the pre-operative period.
Examples: Bendroflumethiazide, Chlorthalidone, Hydrochlorothiazide, Indapamide, Metolozone, Xipamide, bendroflumethiazide + timolol, co-tenidone, Kalspare®, co-amilozide, hydrochlorothiazide + timolol + amiloride, co-flumactone, co-triamterzide
Combination products
Consideration should be given to prescribing the components of combination products as separate medicines perioperatively, but in generalk these drugs should be continued as normal.
Anti-arrhythmics
Class III
These should be continued as normal pre-operatively.
Examples: Amiodarone, Dronedarone
Glycosides
These should be continued as normal pre-operatively.
Example: Digoxin
Anti-anginal
Ivabradine
This should be continued as normal pre-operatively.
Nicorandil
This should be continued as normal pre-operatively.
Ranolazine
This should be continued as normal pre-operatively.
Other
Statins
Continue these in the pre-operative period. If patients are for major vascular surgery, statins should ideally be started at least 2 weeks pre-operatively2.
Examples: Atorvastatin, Fluvastatin, Pravastatin, Rosuvastatin, Simvastatin
Ezetemibe
This should be continued as normal pre-operatively.
Haematology
Background
The following represents an integration of best perioperative practice but should be integrated with any local documents that might apply. For further information, The Beacon Hospital has the following documents available on the Q-pulse system:
- “Pre-op management of anti-coagulation and anti-platelet drugs” (doc. no PPC-ORG-203)
- “Management of direct oral anticoagulants (DOACs)” (doc no. PPC-ORG-204)
Should any questions arise regarding anticoagulants that are not covered by this guide, the above documents should be referred to directly.
If there is any conflict between this guideline and instructions that have been given to the patient, the advice of their specialist takes precedence. It is also advised that the opinion of their consultant surgeon should be sought in the case of such a conflict.
Anti-platelet medications
Aspirin
CARDIAC SURGERY
Alterations to aspirin in this context should be the result of discussions of a multi-disciplinary team including the patient’s surgical, cardiology, and anaesthetic teams3.
NON-CARDIAC SURGERY
high dose (≥150mg OD): Consider reducing to low dose (75mg OD) for 7 days pre-operatively (bleeding risk is lower with 75mg-150mg doses and antithrombotic impact is comparable to higher doses4).
Low dose (≤150mg): Continue this medication pre-operatively EXCEPT
- procedures associated with high risk of bleeding or complications of bleeding5:
- spinal surgery
- ophthalmological procedures
- neurosurgical procedures (craniotomy, transphenoidal procedures)
- individuals who refuse blood transfusion for religious reasons (e.g. Jehovah’s Witness). In this case a consuktant cardiologist should be involved.
ADP Receptor Antagonists
Elective invasive surgery should not be performed on patients who are taking ADP-receptor antagonists. See below for specifics:
CARDIAC SURGERY
Alterations to ADP-receptor antagonists in this context should be the result of discussions of a multi-disciplinary team including the patient’s surgical, cardiology, and anaesthetic teams3.
NON-CARDIAC SURGERY
- If patient has had coronary stenting in the past, or a stroke within the previous 3 months, discuss with pre-operative anaesthetist.
- Invasive surgery should not be performed whilst the patient is taking an ADP-receptor antagonist. If a patient is taking one of these drugs, they should be stopped 5-7 days pre-operatively, and aspirin 75mg OD should be taken in its place.
Examples: Clopidogrel, Prasugrel, Ticagrelor
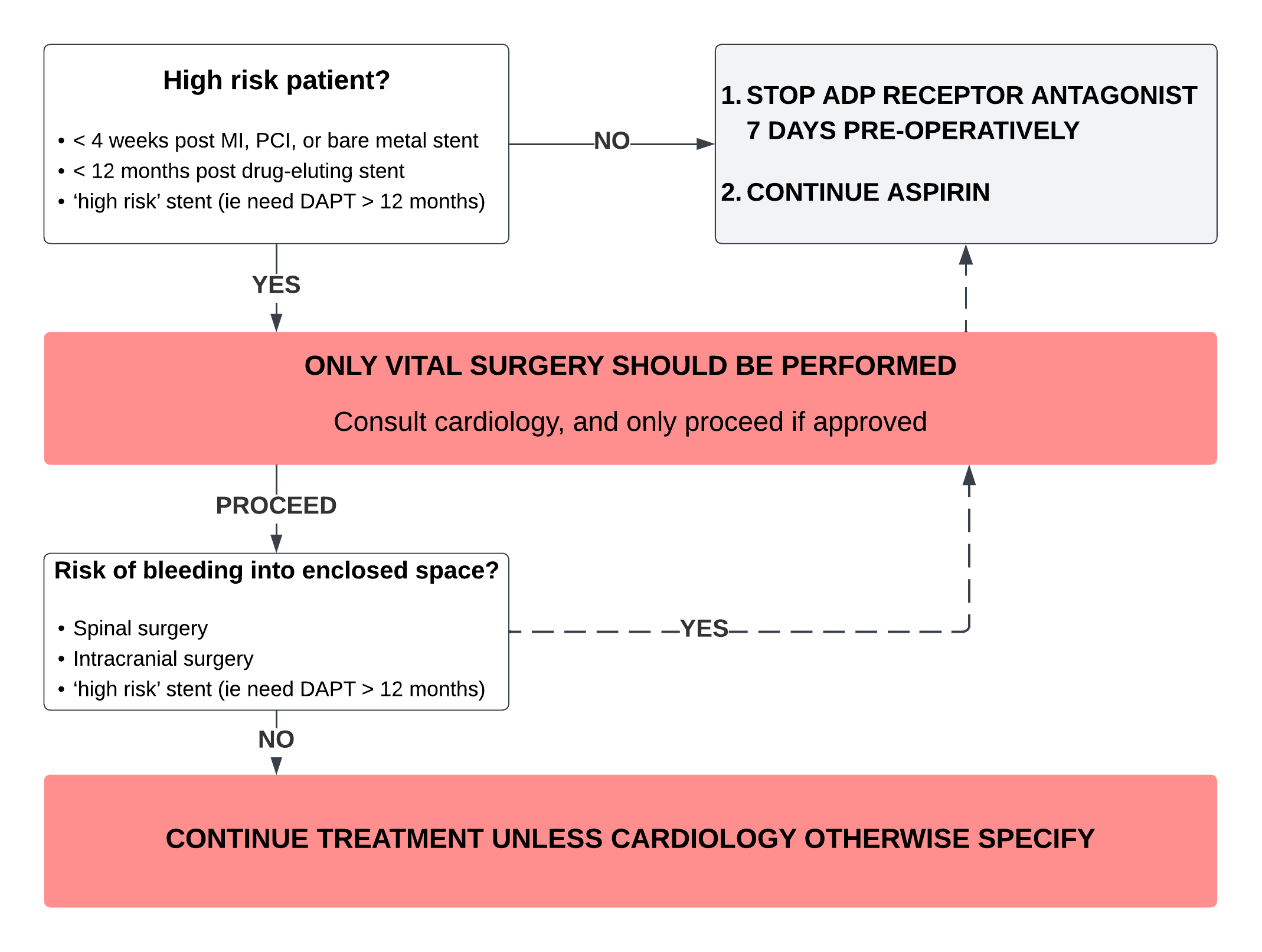
Dual Antiplatelet Therapy (DAPT)
Many patients who are receiving DAPT will be doing so for a specified period of time. These patients are likely to be at high risk of thrombosis, so premature discontinuation if DAPT may lead to significant harm.
The first step in deciding how to proceed is to determine if the patient is at high risk if altering DAPT.
Dypyridamole
Continue this medication pre-operatively, including combination products.
Except procedures associated with high risk of bleeding or complications of bleeding5: - spinal surgery - ophthalmological procedures - neurosurgical procedures (craniotomy, transphenoidal procedures)
In these cases, consider stopping the day before surgery (see Further Information).
Example: Molita® – contains dipyridamole 200mg and aspirin 25mg
Anti-coagulants
The key aspect of managing anti-coagulation around surgery is striking a balance between the risk of thrombosis (in the absence of anti-coagulation) and the risk of bleeding (in the presence of anti-coagulation).
The two main classes of anticoagulation are:
Coumadins
- Warfarin
Dorect Oral Anti-Coagulants (DOACs)
- Rivaroxaban, Apixaban, Edoxaban, Dabigatran
The key issue here is in determining:
how long should the anticoagulant be on hold for pre-operatively (i.e. for how long should the patient not take it)?
does the patient need to be bridged with low molecular weight heparin whilst the anticoagulant is on hold?
Doing this requires knowledge of the indication as to why the patient is taking the medication, the underlying thrombotic risk if the patient is not on anticoagulation, and the patients renal function.
This can be complex, so it is not covered in detail in this section. It is expanded upon in a section about anticoagulation, which can be found here, or located at the far right of the navbar at the top of this webpage.