Stopping anticoagulation and bridging
This section deals with stopping long-term anticoagulation before surgery. It outlines how to determine if a patient needs to stop, for how long they need to stop, and if they need bridged with low molecular weight heparin (LMWH).
Note that if there is any uncertainty or ambiguity, the advice of the anaesthesiologist on call for the clinic, or a consultant haematologist, should be sought.
Overview
The key aspect of managing anti-coagulation around surgery is striking a balance between the risk of thrombosis (in the absence of anti-coagulation) and the risk of bleeding (from the procedure, and in the presence of anti-coagulation).
The two main classes of anticoagulation are:
Coumadins
- Warfarin
Direct Oral Anti-Coagulants (DOACs)
- Rivaroxaban, Apixaban, Edoxaban, Dabigatran
The key issue here is in determining:
how long should the anticoagulant be on hold for pre-operatively (i.e. for how long should the patient not take it)?
does the patient need to be bridged with low molecular weight heparin whilst the anticoagulant is on hold?
Doing this requires knowledge of the indication as to why the patient is taking the medication, the underlying thrombotic risk if the patient is not on anticoagulation, and the patients renal function.
The Approach
A balance between the risk of stopping vs continuing anticoagulation must be sought.
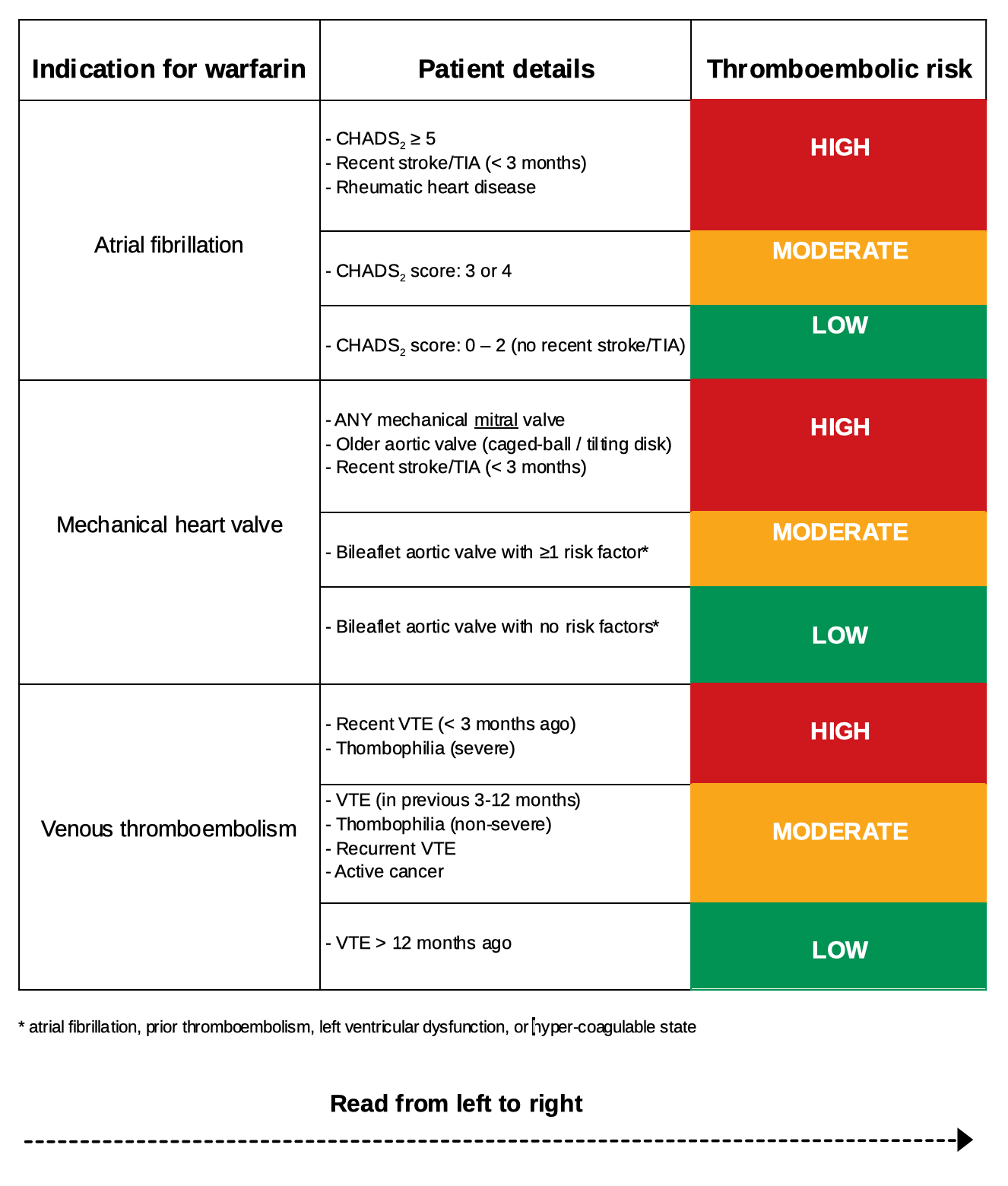
- Determine the thrombotic risk (low/moderate/high)
- the risk associated with stopping anticoagulation (i.e. the thrombotic risk) can be estimated from the following figure (adapted for warfarin use).
- note that is a patient has a combination of low and moderate risk factors, they should be considered high risk.
- the CHADS2 score must be calculated (link here).
Determine the bleeding risk (low/high)
Low bleeding risk procedures include:
minor skin procedures (e.g. basal cell carcinoma resection)
minor hand surgery
cataract excision
diagnostic OGD procedures +/- biopsy (NB polypectomy is high risk)
biliary/pancreatic stenting via endoscopy
diagnostic EUS
Any other procedures should be considered as high risk for bleeding. See here for further details regarding whether the procedure is considered low or high risk for bleeding.
Determine if bridging is needed
- If a patient is at BOTH high thrombotic risk and undergoing a high bleeding risk procedure, they should undergo bridging therapy as outlined below.
- If not, anticoagulants can be stopped as per the timeframes shown below, but LMWH will not need to be prescribed.
Stopping anticoagulation (+ bridging if needed)
Bridging safely involves determining the need for bridging (as above) and then coordinating the time to stop regular anticoagulation with correct timing and dosing of low molecular weight heparin (LMWH). This guide recommends the use of enoxaparin, but other LMWHs are available.
- 1 - Calculate the patients renal function & consequent LMWH dose
- this is important in both determining when to stop regular anticoagulation, and in determining the correct LMWH dose.
- this is calculated by determining the creatinine clearance for the patient (as derived from the U&E taken from their clinic visit).
- a link to allow this to be calculated using the Cockgroft & Gault method can be found here.
- use the table below to determine the dose of LMWH that the patient should take when bridging:
| Renal function (CrCl via C&G) | Dose of enoxaparin (use actual body weight) |
|---|---|
| >30 mL/min | 1mg/kg BD (morning and evening) |
| 15-30 mL/min | 1mg/kg OD (morning) |
| <15 mL/min | 0.5mg/kg OD (morning) |
- 2- Determine when to stop regular anticoagulation
- Warfarin:
- the last dose should be taken on day of procedure -6 (for example if a procedure is on a Friday, the preceding Saturday is the day the lat regular warfarin dose should be taken)
- DOAC:
- see the table for timing of the stop date:
- Warfarin:
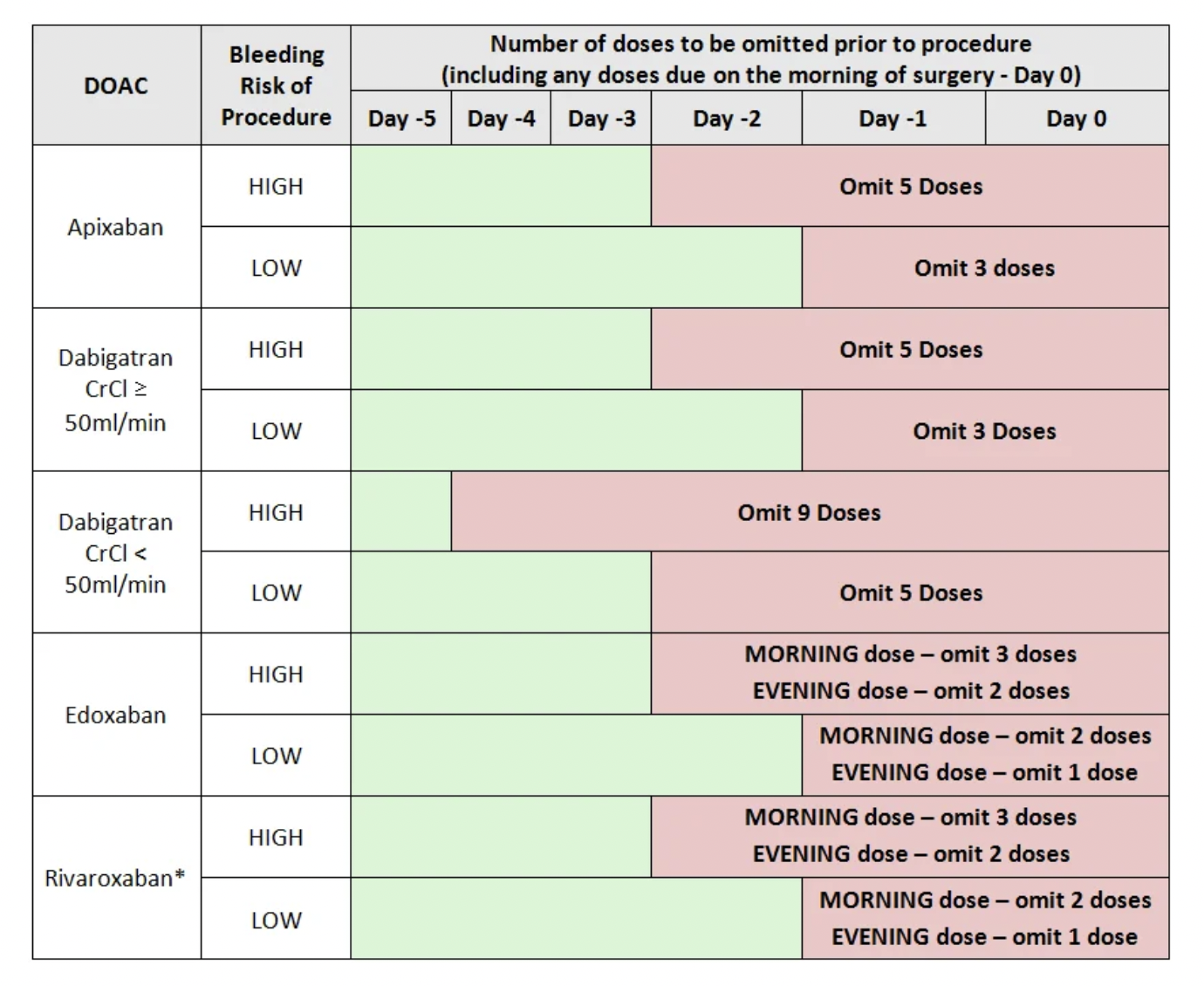
- Low dose Rivaroxaban (2.5mg Twice Daily) is licensed for use in conjunction with aspirin +/- clopidogrel. Refer to individual monographs for the perioperative management of aspirin and clopidogrel and discuss arterial thrombotic risk with a cardiologist or vascular surgeon (depending on indication for therapy). Pre-operative cessation of low-dose rivaroxaban has not been studied and patients should be managed on a case-by-case basis.
- 3 - Determine bridging schedule
- Warfarin:
- day -6: final dose of warfarin pre-op
- day -5: start bridging with enoxaparin (dose as above)
- day -1: test INR (if INR > 1.5, give 1-2mg vitamin K PO) & take morning dose of enoxparin only
- day 0: resume warfarin on evening post-op (if eating/drinking) following confirmation of haemostasis. This can either be at the usual maintenance dose, or double that dose for 2-3 days until INR therapeutic, depending on consultant preference
- DOAC:
- last dose as per above table
- start enoxaparin the day after last dose of DOAC
- day - 1: take morning dose of enoxparin only
- day 0: give prophylactic enoxaparin post-op if haemostasis confirmed. DOAC will generally restart 24-48 hours post-op.
- Warfarin: